Vasectomy is widely regarded as a safe, effective, and permanent form of male contraception. While most patients experience minimal complications, a subset develop localized inflammatory reactions at the vasectomy site. One of the most clinically significant yet often misunderstood complications is sperm granuloma formation. Understanding the mechanisms, clinical presentation, and treatment strategies for this condition is essential for optimizing post-vasectomy outcomes and patient satisfaction.
Understanding Sperm Granuloma Formation After Vasectomy
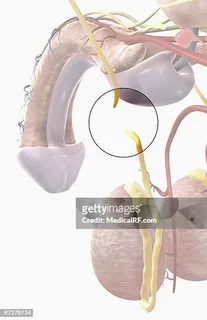
A sperm granuloma is a benign inflammatory mass that develops when sperm leak from the severed ends of the vas deferens into surrounding tissue. Because sperm are antigenic outside the reproductive tract, their presence triggers a localized immune response, leading to macrophage infiltration, fibrosis, and granuloma formation.
In the context of vasectomy, sperm granulomas most commonly develop near the testicular end of the vas deferens, although they may also form at the abdominal end depending on surgical technique and intraluminal pressure dynamics.
While many sperm granulomas are asymptomatic and clinically insignificant, others can cause localized pain, tenderness, or chronic discomfort, prompting the need for targeted treatment.
Pathophysiology: Why Vasectomy Predisposes to Granulomas
After vasectomy, sperm production continues within the testes. With the vas deferens occluded, intraluminal pressure builds in the epididymis and proximal vasal segment. Over time, this pressure may cause micro-ruptures in the vasal wall or epididymal tubules, allowing sperm to escape into surrounding tissue.
The immune system recognizes extravasated sperm as foreign antigens, initiating:
- Macrophage and lymphocyte recruitment
- Formation of multinucleated giant cells
- Collagen deposition and fibrosis
This process culminates in a sperm granuloma, which may function as a “pressure-release valve” in some cases but can also become a source of pain and inflammation.
Clinical Presentation and Diagnosis
Symptoms Associated With Sperm Granulomas
Patients with sperm granuloma formation after vasectomy may present with:
- Localized nodular mass near the vasectomy site
- Tenderness or pain on palpation
- Intermittent scrotal discomfort
- Pain exacerbated by ejaculation or physical activity
In many cases, sperm granulomas are discovered incidentally during physical examination and remain asymptomatic.
Diagnostic Approach
Diagnosis is primarily clinical, based on history and physical findings. Key diagnostic tools include:
- Scrotal examination revealing a firm, mobile nodule
- Scrotal ultrasound to differentiate granulomas from epididymal cysts, tumors, or hematomas
- Doppler imaging to rule out vascular pathology
Biopsy is rarely required unless malignancy cannot be excluded.
Conservative Treatment Strategies
Observation and Reassurance
For asymptomatic or mildly symptomatic cases, no active treatment is required. Many sperm granulomas stabilize or regress over time as inflammation subsides and fibrotic remodeling occurs.
Patient education plays a crucial role, as reassurance can significantly reduce anxiety and symptom perception.
Pharmacologic Management
When symptoms are present, first-line treatment typically involves anti-inflammatory therapy, including:
- Nonsteroidal anti-inflammatory drugs (NSAIDs)
- Short courses of oral analgesics
- Local supportive measures such as scrotal elevation
These interventions aim to reduce inflammation, relieve pain, and prevent progression.
Corticosteroid Therapy
In cases of persistent inflammation, local corticosteroid injections may be considered. These injections suppress immune activity and reduce granuloma-associated edema, often resulting in symptomatic improvement.
Corticosteroid use should be judicious and reserved for patients who fail initial conservative management.
Interventional and Surgical Treatment Options
Nerve-Targeted Pain Management
For patients whose pain appears neuropathic or referred, spermatic cord nerve blocks can provide both diagnostic and therapeutic benefit. Temporary pain relief following a nerve block suggests a neural component to symptoms and helps guide further treatment.
Surgical Excision of Sperm Granuloma
Surgical removal of the granuloma may be indicated in patients with:
- Persistent localized pain
- Failure of conservative and pharmacologic therapy
- Clear correlation between granuloma palpation and symptom reproduction
The procedure involves excision of the granuloma and careful re-ligation of the vas deferens to prevent recurrence. Surgical outcomes are generally favorable when patient selection is appropriate.
Role of Vasectomy Technique in Prevention
The incidence of sperm granuloma formation is influenced by vasectomy technique. Open-ended vasectomy, which leaves the testicular end of the vas unsealed, may reduce epididymal pressure but can increase the likelihood of granuloma formation at the open end.
Conversely, closed-ended techniques reduce sperm leakage but may increase intraluminal pressure. This balance highlights the importance of individualized surgical planning.
Sperm Granulomas and Post-Vasectomy Pain Syndrome
Sperm granuloma formation is closely linked to post-vasectomy pain syndrome (PVPS), a chronic pain condition affecting a small percentage of patients. While granulomas may alleviate pressure-related pain in some cases, they can also act as a chronic inflammatory focus, contributing to persistent discomfort.
Treatment strategies for PVPS often overlap with those used for sperm granulomas, emphasizing multimodal pain management and careful escalation of care.
Patient Counseling and Long-Term Outlook
Importance of Preoperative Counseling
Effective counseling before vasectomy should include discussion of:
- Potential for sperm granuloma formation
- Typical benign nature of granulomas
- Available treatment options if symptoms occur
Transparent communication reduces postoperative anxiety and improves patient satisfaction.
Prognosis
The long-term outlook for patients with sperm granuloma formation is generally excellent. Most cases resolve with conservative management, and surgical intervention is rarely required. When treatment is necessary, outcomes are typically favorable with low recurrence rates.
Future Directions in Treatment and Prevention
Emerging research is exploring:
- Improved vasal occlusion materials to minimize sperm leakage
- Anti-inflammatory coatings for surgical instruments
- Enhanced imaging techniques for early detection
These innovations aim to further reduce the incidence and clinical impact of sperm granuloma formation following vasectomy.
Conclusion
Vasectomy and treatment of sperm granuloma formation represent an important intersection of surgical technique, immunology, and pain management. While sperm granulomas are a known and often benign consequence of vasectomy, symptomatic cases require thoughtful evaluation and a stepwise treatment approach.
From observation and pharmacologic therapy to interventional pain management and surgical excision, effective treatment strategies are available. With proper counseling, early recognition, and individualized care, most patients achieve excellent outcomes and maintain a high quality of life after vasectomy.
FAQs
1. Is sperm granuloma formation dangerous after vasectomy?
No, sperm granulomas are benign inflammatory lesions and are not cancerous. While they can cause discomfort in some patients, they are not dangerous and often resolve with conservative treatment.
2. How is sperm granuloma pain treated after vasectomy?
Treatment typically begins with NSAIDs and supportive care. If symptoms persist, corticosteroid injections, nerve blocks, or surgical excision may be considered depending on severity and response.
3. Can sperm granuloma formation be prevented during vasectomy?
While it cannot be completely prevented, careful surgical technique, appropriate vasal occlusion methods, and proper postoperative care can reduce the likelihood and severity of sperm granuloma formation.
If you’d like, I can also:
- rewrite this in a more academic or journal-style tone,
- optimize it for SEO keyword density, or
- create a clinical illustration outline or table summary for publication.